ECG Changes In Pulmonary Embolism: What You Need To Know
Let’s talk about ECG changes in pulmonary embolism because it’s a big deal, and you might not even realize how important it is. Imagine this: you’re in the ER, feeling short of breath, with chest pain, and your heart is racing. The doc hooks you up to an ECG, and boom—there’s something funky going on. That’s where understanding ECG changes comes into play. It could be the key to catching pulmonary embolism early, and we all know early detection can save lives. So, buckle up, and let’s dive into this topic.
Pulmonary embolism (PE) is no joke. It’s like a traffic jam in your lungs, but instead of cars, it’s blood clots blocking the flow. And when it comes to diagnosing PE, the ECG can be your best friend—or your worst enemy, depending on how you interpret it. That’s why we’re here: to break it down for you in a way that makes sense.
Now, don’t get me wrong. The ECG isn’t the definitive test for PE, but it can give you some serious clues. And in the world of medicine, every clue counts. So, whether you’re a healthcare professional or just someone curious about how the body reacts to PE, this article’s got you covered.
- Damon Albarns 90s The Era That Redefined Music And Culture
- Dandelion Wishes Candle Co Your Ultimate Guide To Ecofriendly And Luxurious Candles
Understanding Pulmonary Embolism
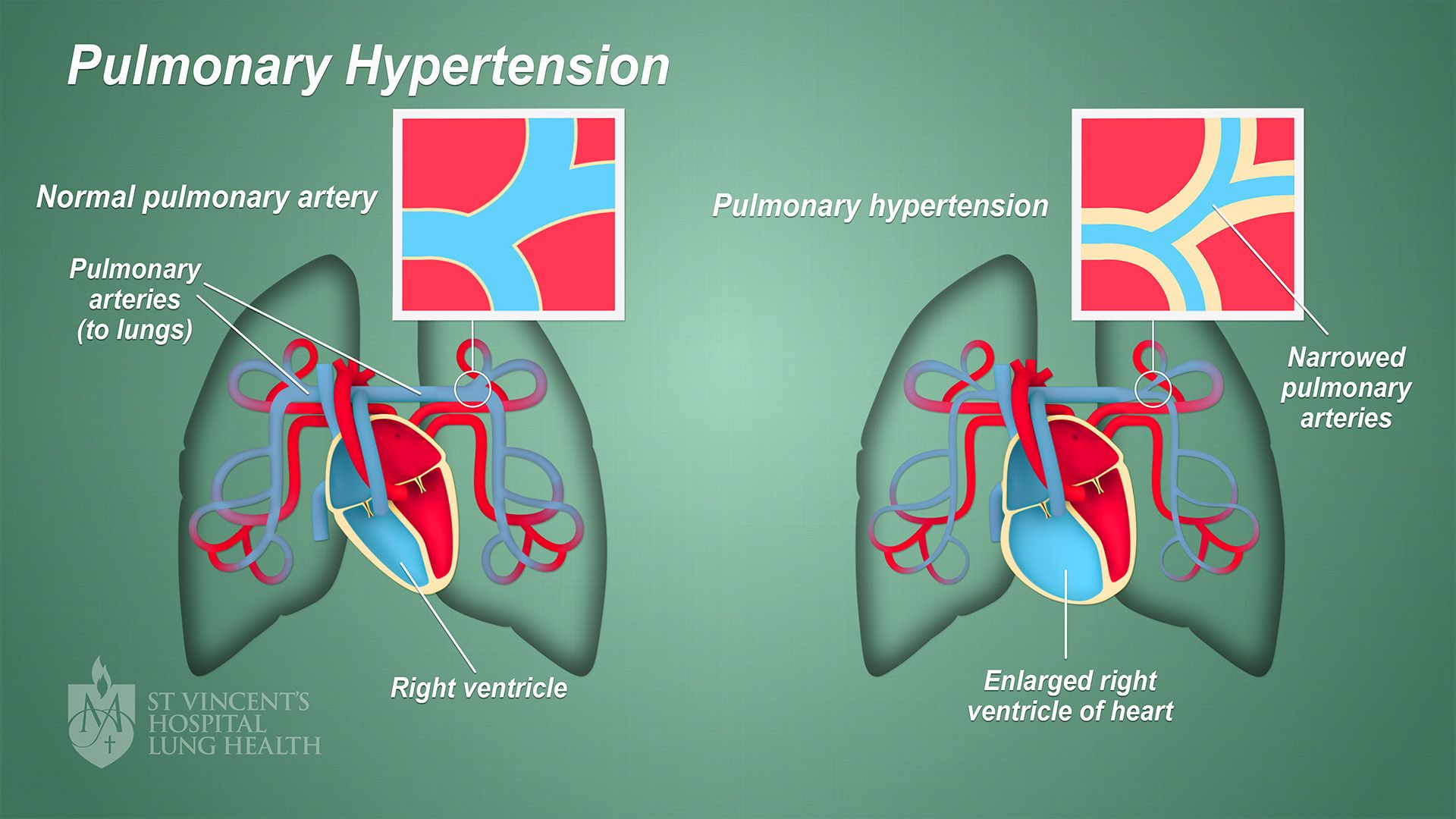
Before we dive deep into the ECG changes, let’s first understand what pulmonary embolism is all about. Think of it as a blockage in the pulmonary arteries in your lungs, usually caused by blood clots that travel from somewhere else in your body—most commonly the legs. And trust me, it’s not a party you want to attend.
PE can cause a range of symptoms, from mild discomfort to life-threatening conditions. And here’s the kicker: sometimes, the symptoms can be so vague that they get mistaken for something else entirely. That’s why having tools like the ECG to help guide diagnosis is crucial.
Causes and Risk Factors
So, what causes pulmonary embolism? Well, it’s usually a blood clot that travels from the deep veins of the legs or pelvis. But let’s not forget the risk factors that make you more susceptible:
- Prolonged immobility—like sitting on a long flight
- Surgery or trauma
- Certain medical conditions like cancer or heart disease
- Family history of blood clots
- Smoking
- Obesity
See, it’s not just one thing that causes PE. It’s a combination of factors that can stack up and increase your risk. And that’s why being aware of these risk factors is so important.
ECG Changes in Pulmonary Embolism
Alright, let’s get to the good stuff. What exactly are the ECG changes you might see in pulmonary embolism? Well, it’s not always straightforward, but there are some patterns that doctors look out for. And here’s the thing: these changes can vary from person to person, so it’s not a one-size-fits-all kind of deal.
One of the most common ECG findings in PE is sinus tachycardia. That’s when your heart rate speeds up, and it’s the body’s way of saying, “Hey, something’s not right here.” But that’s not all. You might also see signs of right ventricular strain, which is like the heart saying, “I’m working overtime to pump blood through those blocked arteries.”
Sinus Tachycardia
Sinus tachycardia is like the canary in the coal mine for pulmonary embolism. It’s a sign that your body’s trying to compensate for the lack of oxygen in the blood. And while it’s not specific to PE, it’s definitely something that raises a red flag.
Now, here’s the kicker: sinus tachycardia can also be caused by other things, like anxiety or fever. So, just seeing it on an ECG doesn’t automatically mean you’ve got PE. But when combined with other symptoms and risk factors, it’s definitely worth investigating further.
Right Ventricular Strain
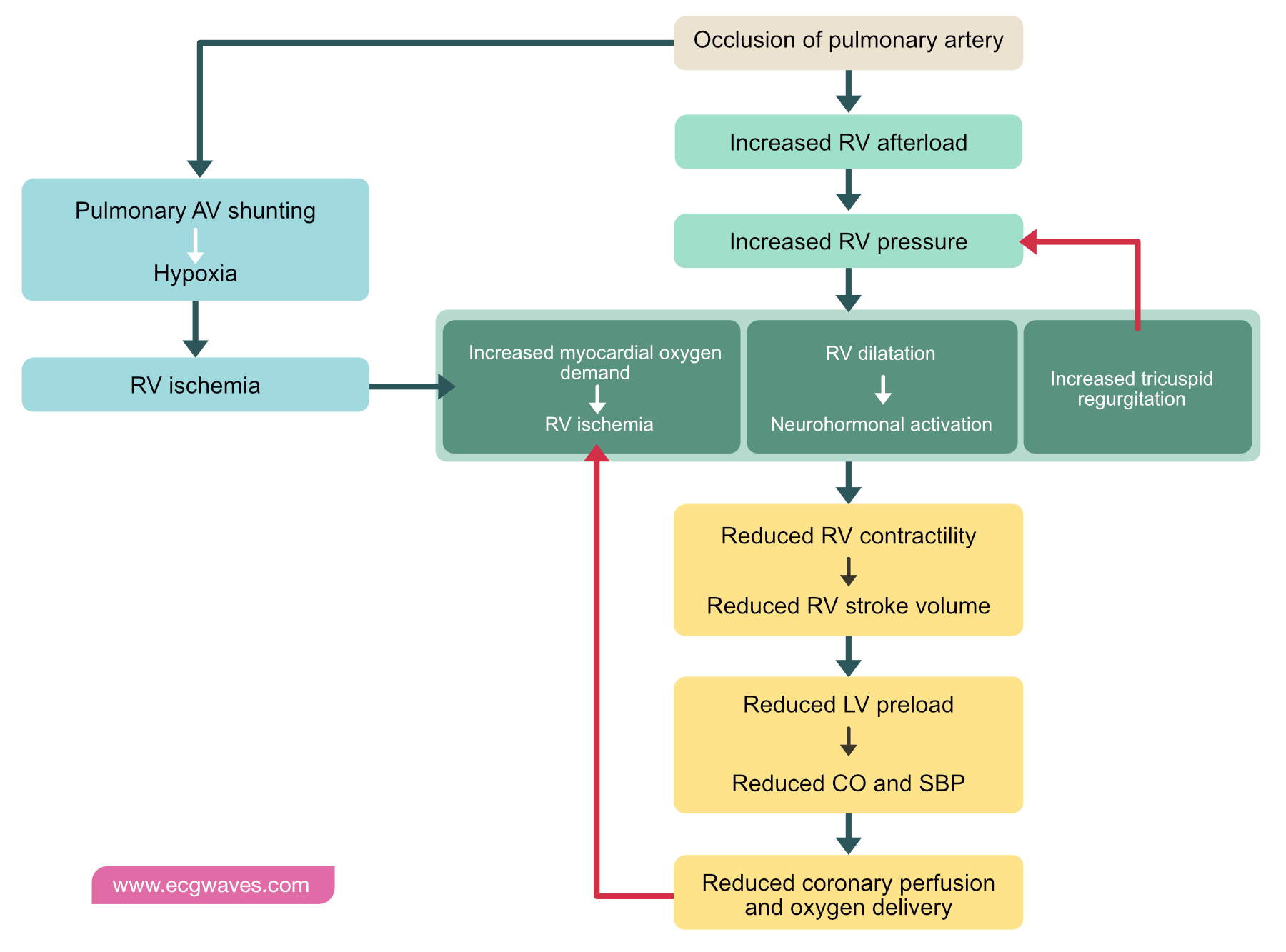
Right ventricular strain is another biggie when it comes to ECG changes in pulmonary embolism. It’s like the heart saying, “I’m under pressure here.” And that pressure comes from the blockage in the pulmonary arteries, which makes it harder for the right side of the heart to pump blood through.
On an ECG, you might see signs like inverted T waves in the right precordial leads (V1-V4), or even an S1Q3T3 pattern, which is a fancy way of saying there’s a deep S wave in lead I, a Q wave in lead III, and inverted T waves in lead III. And while these findings aren’t always present, they can be pretty telling when they are.
ST Segment Changes
ST segment changes can also occur in pulmonary embolism, and they’re usually indicative of right ventricular ischemia. That’s when the heart muscle doesn’t get enough oxygen, and it’s not a good sign. You might see ST elevation or depression, depending on the severity of the blockage.
And here’s the thing: ST segment changes can mimic other conditions, like a heart attack. So, it’s important to look at the whole picture, not just one part of the ECG, to make an accurate diagnosis.
ECG Patterns in Pulmonary Embolism
Now, let’s talk about some of the specific ECG patterns you might see in pulmonary embolism. Remember, these patterns aren’t always present, but when they are, they can be pretty telling. So, let’s break it down:
- S1Q3T3 pattern
- Inverted T waves in V1-V4
- ST segment changes
- Sinus tachycardia
Each of these patterns tells a different story, and when you put them all together, you get a clearer picture of what’s going on in the heart and lungs.
S1Q3T3 Pattern
The S1Q3T3 pattern is one of the more classic ECG findings in pulmonary embolism. It’s characterized by a deep S wave in lead I, a Q wave in lead III, and inverted T waves in lead III. And while it’s not always present, when it is, it’s a pretty good indicator that something’s up.
But here’s the thing: the S1Q3T3 pattern can also be seen in other conditions, like right bundle branch block. So, again, it’s important to look at the whole picture, not just one part of the ECG.
Diagnosing Pulmonary Embolism
ECG changes are just one piece of the puzzle when it comes to diagnosing pulmonary embolism. You’ve also got to consider things like symptoms, risk factors, and other diagnostic tests. And that’s where the fun begins.
Some of the other tests that might be used to diagnose PE include D-dimer tests, CT pulmonary angiography, and ventilation-perfusion scans. And while the ECG can give you some clues, it’s not the definitive test. That’s why it’s so important to use it in conjunction with other tests.
Role of D-dimer Test
The D-dimer test is like the sidekick to the ECG when it comes to diagnosing pulmonary embolism. It measures a protein fragment that’s released when a blood clot breaks down. And while it’s not specific to PE, it can help rule out the condition in low-risk patients.
But here’s the thing: the D-dimer test can also be elevated in other conditions, like infection or inflammation. So, again, it’s not a definitive test on its own, but it can be a helpful tool when used in conjunction with other tests.
Treatment Options
Now that we’ve talked about diagnosing pulmonary embolism, let’s talk about treatment options. And let me tell you, there are plenty of ways to tackle this condition, depending on the severity and the patient’s overall health.
Anticoagulants, or blood thinners, are usually the first line of treatment for PE. They help prevent the clot from getting bigger and reduce the risk of new clots forming. And in severe cases, thrombolytic therapy might be used to dissolve the clot quickly.
Anticoagulants
Anticoagulants are like the superheroes of PE treatment. They don’t actually break down the clot, but they do prevent it from getting bigger and reduce the risk of new clots forming. And while they’re usually pretty effective, they do come with some risks, like bleeding.
So, it’s important to weigh the benefits and risks before starting anticoagulant therapy. And that’s where the expertise of your healthcare provider comes in.
Prevention Strategies
Preventing pulmonary embolism is all about reducing your risk factors. And while some risk factors, like family history, are out of your control, there are plenty of things you can do to lower your risk.
Staying active, avoiding prolonged immobility, and managing underlying health conditions are all great ways to reduce your risk of PE. And if you’re in a high-risk situation, like after surgery, your doctor might recommend prophylactic anticoagulants to prevent clots from forming.
Compression Stockings
Compression stockings are like the unsung heroes of PE prevention. They help improve blood flow in the legs and reduce the risk of blood clots forming. And while they might not be the most fashionable accessory, they’re definitely worth considering if you’re at risk for PE.
Conclusion
So, there you have it. ECG changes in pulmonary embolism are an important piece of the diagnostic puzzle, but they’re not the whole picture. It’s all about looking at the big picture and using a combination of tools to make an accurate diagnosis.
And remember, prevention is key. By managing your risk factors and staying informed, you can reduce your chances of developing pulmonary embolism. So, take action, stay healthy, and don’t hesitate to reach out to your healthcare provider if you have any concerns.
Feel free to leave a comment or share this article with someone who might find it helpful. Knowledge is power, and the more we know, the better we can take care of ourselves and our loved ones.
Table of Contents
- Understanding Pulmonary Embolism
- ECG Changes in Pulmonary Embolism
- Right Ventricular Strain
- ECG Patterns in Pulmonary Embolism
- Diagnosing Pulmonary Embolism
- Treatment Options
- Prevention Strategies
- Conclusion

Detail Author:
- Name : Carson Collins
- Username : jasmin76
- Email : jeffery.nader@gmail.com
- Birthdate : 2003-10-13
- Address : 1710 Gerhold Drive Lake Hertha, DE 02283
- Phone : +1-520-721-8066
- Company : Williamson-Baumbach
- Job : Animal Scientist
- Bio : Minus quis et cum amet. Perferendis nemo et in et quaerat dolorum optio dolor. Quae quia tempore expedita dolores voluptates.
Socials
tiktok:
- url : https://tiktok.com/@jaufderhar
- username : jaufderhar
- bio : Numquam quisquam natus quae id blanditiis quia qui blanditiis.
- followers : 1048
- following : 2185
facebook:
- url : https://facebook.com/aufderharj
- username : aufderharj
- bio : Et vel qui nesciunt modi. Dolorum quos qui saepe rerum.
- followers : 2587
- following : 836
instagram:
- url : https://instagram.com/aufderharj
- username : aufderharj
- bio : Voluptas quia molestiae aspernatur nisi. Ut velit sed id cupiditate quis dolores consequatur.
- followers : 1815
- following : 1215